
During the last year of my Northeastern University (NEU) BSEE experience, I had to complete a Capstone. A capstone project is a culminating, integrative project that students undertake and is designed to apply and synthesize the knowledge and skills acquired throughout the BSEE program. The Key characteristics, or goals, of a capstone project include:
- Integration of Knowledge: The project required me to draw upon the various concepts, principles, and technical skills I have learned during my coursework to solve a real-world engineering problem and address a specific engineering challenge. That what the Infant Safety And Vitals Evaluation Device (iSaved) project was all about. Infant Mortality Rate (IMR) is the probability rate of dying between birth and the age of 1 year old (expressed as deaths per 1,000 births), and the iSaved project designed, and almost fully created a product for that.
- Interdisciplinary Approach: The Capstone project encouraged interdisciplinary collaboration. Students may work in teams, bringing together their expertise in electrical engineering with knowledge from other fields to address complex, multifaceted problems. The iSaved Capstone project team members included Eric Davis, Kyle DeGhetto, Mohamed El-Toukhy, Lisa Paz, and Michael Silverman.
- Practical Application: The iSaved project was a practical and application-oriented, aiming to produce a tangible solution, design, and a prototype that had real-world relevance and impact.
- Mentorship: Our team worked closely with closely with Waleed Meleis, a faculty mentor, who provide us with guidance and expertise throughout the project’s duration.
- Presentation and Communication: The capstone project culminated in a formal presentation and a report in which we presented our findings, methodologies, and outcomes to faculty, and peers.
- Assessment: The project was assessed based on its technical merits, problem-solving effectiveness, creativity, and the ability to communicate and defend the project’s outcomes and decisions. Guess what – we pass!
The specific details and requirements of the iSaved capstone project are outlined below, and are a direct copy/paste of the iSaved proposal paper.
Abstract
The Infant Mortality Rate (IMR) is the probability rate of an infant dying between birth and the age of 1 year old (expressed as deaths per 1,000 births). The estimated IMR for 2012 in the USA is about 5.98% [1]. This is translated to an estimate of 254,000 yearly deaths [2], out of which over 2,200 will be due to Sudden Unexplained Infant Death Syndrome (SUIDS). This statistical value makes SIDS the third most common death among infants under one year old. One third of those deaths are caused by Sudden Infant Death Syndrome (SIDS).
In order to monitor babies safely there are various audio, video, and motion monitors in the market. These monitoring systems fail in providing the true information that parents seek: gain live-time knowledge of their baby’s vital signs. That is where the Infant Safety And Vitals Evaluation Device (iSAVED) comes to play. iSAVED utilizes photoplethysmography (PPG) analysis methods in order to detect the cardio-vascular pulse waves traveling through the body.
iSAVED illuminates the skin with white color LED and then measures the reflected pulse wave. By computing the standard deviations and intensities of the red (R), green (G), and blue (B) color bands of the pulse waves, we are able to obtain the level of oxygenated hemoglobin in the blood (PaO2) and heart-rate (HR). This method is based on the fact that blood absorbs light more than the surrounding tissue [3]; due to hemoglobin’s (Hb) red color its absorption spectra helps to quantify the levels of Hb in the blood. In addition, this method is used to measure the change in volume of the perfused blood in the subcutaneous tissue of the skin, by analyzing the RGB absorption and reflection intensities. Analysis of these changes allows us to compute the HR [4].
Through the course of our device development we were able to successfully implement the cellphone application, base station, and the hardware for the jumpsuit. Unfortunately due to time restrictions we were unable to fully implement the signal processing algorithms needed to extract the vital signs from the sensor data. Additionally, it was found that the sensor system used was not ideal, and that a different sensor design is likely needed to fully implement the project.
Introduction and Related Work
Although medicine was able to extend the life expectancy of the average American from about 68 to 78 years [1], it has only managed to drop the Infant Mortality Rate (IMR) from about 30% to 7% [2] in the past 60 years. The three leading causes of infant death are: congenital malformations, low birth weight, and sudden infant death syndrome [3]. Sudden Infant Death Syndrome (SIDS) is a term that describes the sudden death of an infant under the age of 1 year. Although SIDS claims the lives of about 3000 babies each year, the cause of SIDS remains unknown to physicians and other professionals in the field. No obvious cause can be found even after a complete after-death investigation is conducted. Doctors believe that SIDS happens quickly with no signs of suffering or pain, yet investigations such as autopsy, review of prior to death symptoms, and medical history, fail to shed light on a cause [4].
SIDS is the only unknown cause of Sudden Unexpected Infant Death (SUID). SUIDs claim about 4500 lives each year. The leading causes of SUIDs are: SIDS, suffocation, hyper or hypothermia, neglect and homicide infections, metabolic disorders, cardiac channelopathies, and poisoning [5].
The unknown death factors of SIDS and the fact that medical examiners are classifying SIDS as ‘accidental suffocation’ or ‘unknown cause’ forced the Centers for Disease Control and Prevention (CDC) to establish the “Sudden Unexpected Infant Death Initiative”. Some of the goals of this initiative are to standardize and improve data collected at death scene and to reduce SUID by using improved data to identify those at risk [6].
As of today there are a few educational programs such as the “Back to Sleep” campaign led by the National Institute of Child Health and Human Development (NICHD) and the National Black Child Development Institute (NBCDI) [7]. Such campaigns are aimed to educate parents, and the general public, about the myths and facts behind SUIDs and how to try and prevent them. However, because SUIDs occur when the parents or guardians are least expecting it, it is vital to constantly monitor the infant’s vital signs. As of today, the popular and widely used baby monitors are inefficient and unreliable at fulfilling the task at hand, and really saving infants lives. They include various combinations and setups of sound, video, and motion detectors. The following list represents the chosen top competing products among those that were reviewed:
- Summer Infant Slim & Secure Digital Handheld Color Video Monitor by Summer Infant. This baby monitor is basically a handheld color video monitor that offers parents a video monitor for around-the-clock check-ups on baby. It is sold for $199.99 [8]
- Angelcare Movement Sensor with Sound Monitor by Angelcare. This baby monitor is a sound and movement monitor composed of three main pieces: video, sound, and a movement monitor. The under the mattress pad is used to detect the baby’s movement and will sound an alarm if the baby has not moved for 20 seconds, or release ‘tic’ sounds when the baby is moving. In addition, this baby monitor has the typical baby sound monitor. It is sold for $79.99 [9]
- Tommee Tippee Closer to Nature Digital Video Sensor Pad Monitor by Tommee Tippee. This specific baby monitor is a combination of all three monitoring techniques of audio, video, and motion. It uses a motion pad, video camera, and microphone/speaker system. It is all packed at the price of $299.99 [10]
Upon reviewing the capabilities of these products, a few important issues were raised:
- If the baby is suffocating, the parents will not know about it until the motion alarm goes off.
- In the sever case when an infant is choking, the pad will detect motion until the infant passes out from lack of oxygen supply. The audio sensor will not detect any alarming sounds because the baby is suffocating and is not able to produce sound. Consequently, the monitoring system will fail to alarm the parents and the baby may suffer brain hypoxia, because the brain cells in an infant are very sensitive to lack of oxygen and will start dying in minutes after the oxygen supply disappears [11].
- If the motion detector is under sensitive, the alarm will sound around every 20 seconds.
- If the motion sensor is over sensitive, it will detect motion which may not be caused by the baby, but by its crib or surrounding environment.
- The motion sensor pad can be used only with the crib. It cannot be used in any different environment.
- In the video feed feature of the baby monitor, parents do not see clearly whether the baby is not moving because it is sleeping, or because it has stopped breathing.
We proposed and designed the “Infant Safety And Vitals Evaluation Device”, in short iSAVED. iSAVED was designed to overcome these shortcomings by providing an accurate, immediate, and portable solution for monitoring a baby’s vital signs. iSAVED constantly monitors and report oxygenated hemoglobin levels in the blood stream, as well as heart-rate and respiratory-rate. iSAVED was supposed to utilize a sophisticated combination of advanced imaging and complex signal processing algorithms to provide parents with the ability to monitor, in real time, their baby’s vital signs. The obvious strength points w iSAVED were that it does not rely on motion, sound, or video feed from the baby, it is non-invasive, and provides a live update about the baby’s condition. In addition, iSAVED provides a radio free monitoring environment. Although the prototype costs were high, it is possible to lower the final production costs by designing and building the various systems in house and not buying pre-built modules.
In addition to the novel monitoring system, iSAVED is centralized around the baby’s health care and therefore aims to maintain a radiation free environment. In order to achieve this goal iSAVED utilizes a unique combination of infrared and Bluetooth communication systems. The acquired data is sent via I2C from the sensor to a Digital Signal Processor (DSP). The DSP analyzes the data and transmits it via infrared to a distant device, the base-station. The base-station receives the infrared data and further analyzes it and transmits it to an Android based device using Bluetooth protocol. This method was chosen in order to lower costs and utilize devices such as smartphones and tablets, most parents already have in their homes (about 55% of all new smartphone buyers went with Android [16]). The Android based application provides all the information about a baby’s vital signs and it sound an alarm if anything goes wrong.
Design Specifications
iSAVED is a wireless medical device that uses recently discovered technology to monitor an infant’s vital signs. This device informs the parents or guardian through a smart phone application, if there are any abnormalities in the child’s Heart Rate, Respiratory Rate, or Blood Oxygen Level (SPO2), both visually and through an audible alarm.
he iSAVED consists of two main devices. The first device is the Portable Safety Garment, which shall be referred to as the Jumpsuit. The Jumpsuit is worn by the infant, and the electronics are encased in two separate pouches, which allow the electronics to be removed from the baby’s garment for laundering. Unlike invasive vital monitoring systems, the Jumpsuit acquires the signals through the use of image sensors placed against the skin, which in turn eliminates the risk of electric shock. The collected data is transmitted to the Base-Station receiver through infrared (IR) light. This method was chosen because, unlike radio communication such as Bluetooth or Wi-Fi, the IR transmitter avoids concerns over the possibility of dangerous radiation exposure. The Jumpsuit is powered by a rechargeable Lithium Polymer (LiPo) battery.
The Base-Station will provide a communication channel between the Jumpsuit and the smartphone application. It will be positioned above the crib, at a distance that eliminates the possible absorption of dangerous levels of electromagnetic radiation. This device is responsible for relaying the data from the Jumpsuit to the smartphone via Bluetooth. The microcontroller is responsible for relaying the data received from the IR receiver, and processing the data to determine if there is an anomaly for any of the vitals that would necessitate an alarm, and then relaying the vitals and alarm data to the smartphone via Bluetooth. The Base-Station will be powered by a 7.5VDC power supply.
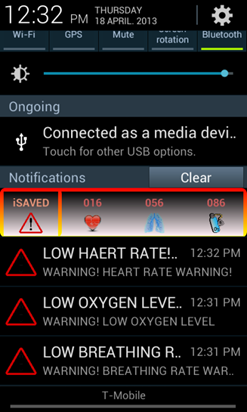
The iSAVED smartphone application will provide the parents a comforting and aesthetic visual that shows their child’s vitals in real-time, as well as alerts the parents to any abnormalities in these vitals. The data will be sent to the Android smartphone via Bluetooth, with a range up to 100m. The application will display the child’s Heart Rate Breathing Rate, and Blood Oxygen Saturation Level, updated every second. In case of a detected anomaly, a message is provided as a visual alert in the notification bar, the phone will highlight the graph of the affected vital in the open application, the display LED light will be lit if available, and an audible alarm will be triggered on the parent’s phone, prompting the parent to check on their child.
The iSAVED device is intended to be operated in the infant’s home. Certain communication limitations arise when using the transmitter/receiver outdoors or when placed in separate rooms, as the Jumpsuit must be within the line of sight of the receiver. Bluetooth is required in order to view the graphs and vital statistics in real-time on a smartphone. There are inherent range limitations with Bluetooth. The battery life in the vest requires recharge, and lasts approximately 40 hours.
Design Overview
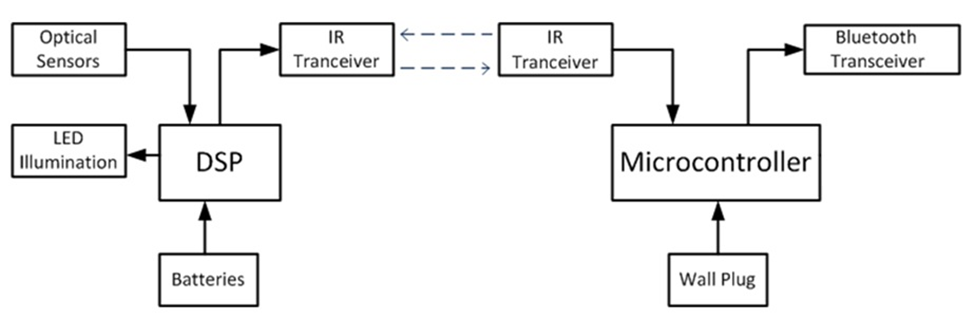
iSAVED contains two systems, the Jumpsuit and the Base-Station. An infant will be wearing a garment with a pair of built-in pockets which host the optical sensors and DSP. The optical sensors are placed next to a white LED which is used to illuminate the skin. The sensor provides 16-bit data values of the intensities of the green, red, and blue light color band spectrums. This information travels to the DSP over a wired I2C communication channel, where it will be processed using complex algorithms in order to computer the oxygen saturation levels, heart rate, and respiratory rate of the baby. The battery life of the Jumpsuit must be extended as long as possible so two rechargeable lithium polymer batteries are used with a working life time of over 40 hours. The DSP sends the processed data to an IR transmitter which is linked with the Base-Station wirelessly.
An IR receiver on the Base-Station must be located within the line of sight of the transmitter on the infant. The information from the Jumpsuit is received through an IR transceiver and sent to the microcontroller via a serial UART channel. This microcontroller then classifies the data and transmits the received signals along with alarm states via Bluetooth to an android device within range. The Android phone application then displays the baby’s heart rate, respiratory rate, and blood oxygen level. In addition, this application sounds alarms to alert the parent if there are any abnormalities with their baby’s vitals.
Design Details
Portable Safety Garment

Sensor Array
The sensor system we implemented consists of an LED for illumination combined with a TAOS TCS3471 digital RGB color sensor. These sensors were selected due to a number of factors. The TAOS sensors are capable of sampling a separate Red, Green, Blue, and Clear channel at up to 400kHz and transmitting this information as a digital measurement using the I2C communication protocol. For our design we chose to use these sensors instead of a digital camera due to their much higher sampling rates as well as our assumption that they would simplify some of the processing described in [17] to extract the important physiological parameters. The sensors were combined with a white LED for illumination and a circuit was built to allow for easy testing with the use of an adult volunteer. The sensor circuit was attached to a flexible arm band to facilitate this testing; the arm band can be seen in Figure 2 above.
As we began to implement the signal processing algorithms we discovered that our choice in implementing these sensors was not optimal. With additional time we feel it would be possible to replace these sensors with either a high-speed digital camera, or a larger array of color sensors.
Signal Processing
The inspiration for our project came from the research outlined in [17]. The premise involves analyzing the Red-Green-Blue (RGB) output of an optical sensor or camera in order to calculate the current heart rate, breathing rate, and approximate blood oxygen saturation (SpO2).
Due to time constraints, we were unable to fully implement the signal processing as proposed. Limited progress was made in implementing the algorithm for calculating the blood-oxygen level and heart rate, but complete and successful parameter extraction was not realized. The details of the parameter extraction algorithms we had planned to implement can be found in [17], [18], [19], and [20].
To estimate the SpO2 level of the infant we attempted to implement an algorithm similar to what is used in traditional pulse oximeter. The algorithm was adapted to an RGB sensor as outlined in [17] and then modified slightly for our application. The equation used to calculate oxygen saturation is given in [17] as:
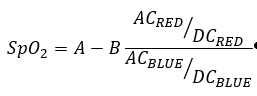
In [17] the constants A and B are selected by setting the initial SpO2 to the measurement obtained by a commercial pulse oximeter. In our testes we attempted to compare the output of the algorithm with a store bought pulse oximeter, but we found the purchases product to be unreliable and inaccurate. During testing we selected parameters A and B by trial and error in an attempt to keep the data within a range that could be easily dealt with in the DSP and transferred over the IR communication link. We were able to implement a version of this algorithm that would work intermittently during testing, but as described in the section on the sensor above, we believe that the use of a single sensor of the type we proposed was not sufficient to provide the data needed to correctly extract the vital signs.
In order to extract the heart rate and breathing rate, the real time intensity of the green channel from the optical sensor should be used. As described in [17], the green channel is selected due to its high level of absorption by hemoglobin in the blood. In order to extract the heart rate we had planned to use a beat detection algorithm as described in [20], and for the breathing rate we had planned to implement the variable frequency complex demodulation algorithm as explained in [18] and in more detail in [19].
Digital Signal Processor
To perform the onboard signal processing we have chosen to implement Microchip’s dsPIC33fj256GP70A Digital Signal Processor. This DSP has a 16-bit memory hierarchy with a built in UART and I2C communication channel. It is also capable of computing 40 Million instructions per second. The processor can be programmed using the MP Lab supplied C IDE and was available in a development board format for easy use during initial testing and prototype construction.
Infra-red Transmitter
In order to safely transmit wireless information we have chosen to incorporate infra-red (IR) transmission from the device to the wireless base-station. This will serve two primary safety goals; to avoid any concerns over strangulation from wires, and to avoid concerns over possible radiation effects of transmitting a wireless signal from a device worn by an infant.
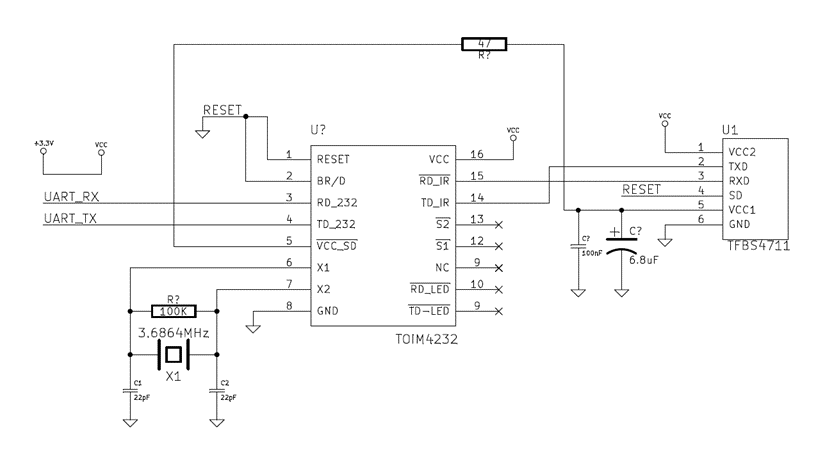
The circuit that we utilized consisted of an infrared transceiver IC and an IrDA endec IC (encoder and decoder). This circuit communicated over the UART bus which allowed for easy interface to the mBed and the DSP. As a transceiver the same circuit could be used at both devices for two way communication. The configurable circuit was designed to use an IrDA bitrate of 9.6kB/s. IrDA stands for Infrared Data Association, which is a standard protocol for infrared communication. Within the endec, an automatic pairing sequence occurs when the devices are turned on. At this point the endec was used as a simple UART terminal where data was sent and received. In experimental testing we achieved accurate communication at a distance of 15 feet.
We used a Vishay TFBS4711 transceiver and a Vishay TOIM4232 endec. These matched components allowed for simple integration between the transceiver and the endec.
Packaging
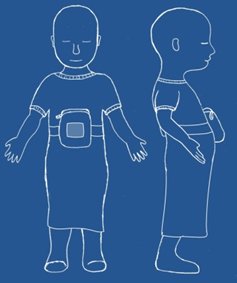
Safely and comfortably containing the electronics within the vest is a primary concern. The designed solution to this is having a special jumpsuit that contains pouches to encase the iSAVED electronics, allowing easy removal of the electronics. The jumpsuit was designed as a a baby gown, which allows for the garment to be pulled over the infants head for easy dressing. It has two arms, and is opened at the bottom.
The jumpsuit contains two pouches, both an inner and outer pouch. Both pouches open at the top and can be securely closed with snap fasteners. Each pouch also adorns a thin mesh center that allows sufficient openings within the garment to allow the small sensor surfaces an unobstructed line of sight with the infant’s skin. These openings also allow the data transmission from the DSP to the base-station via IR transmitter. In addition to this, the pockets will be water resistant to protect against sweat, or if the baby soils itself. Finally, the jumpsuit has an elastic, adjustable belt that allows for the electronics to be secured properly.

The iSAVED electronics core will be easily removable from the iSAVED Jumpsuit in order to allow it to be laundered when soiled. This will also let the user purchase only one set of electronics which can be installed into different garments as desired, and will allow the product to be used continually as the child grows without unneeded expense.
Power System

Among the many things that were considered while selecting a suitable power source, for the electronics within the jumpsuit, include: mobility, lightweight, small size, recharge-ability, and sufficient battery life for at least 24 hours of continuous operation. A perfect candidate for meeting all these specifications was the SparkFun 3.7V 2000mAh Lithium Polymer Li-Po Battery shown in Figure 6. The Li-Po battery is small in size, with dimensions of 0.25″ x 2.1″ x 2.1”, and only weighs 36g. Two of these batteries were connected in series and combined together in a single battery pack. The battery packs are swappable which will enable parents to exchange them when one is out of charge, and will ensure the continuous use of the jumpsuit.
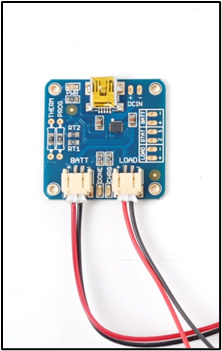
Li-Po batteries require special charging circuits. The Adafruit Li-Po USB Charger was used, and is shown in Figure 7. The Charger circuit is connected to a computer via a mini-USB connector for charging. The other two terminals are for the battery and the electric load to be connected with standard JST cables. This allows the load to still be fed and continue its operation while the battery is being charged. However, the end user will be clearly advised that it is unsafe to charge the battery while the infant is wearing it.
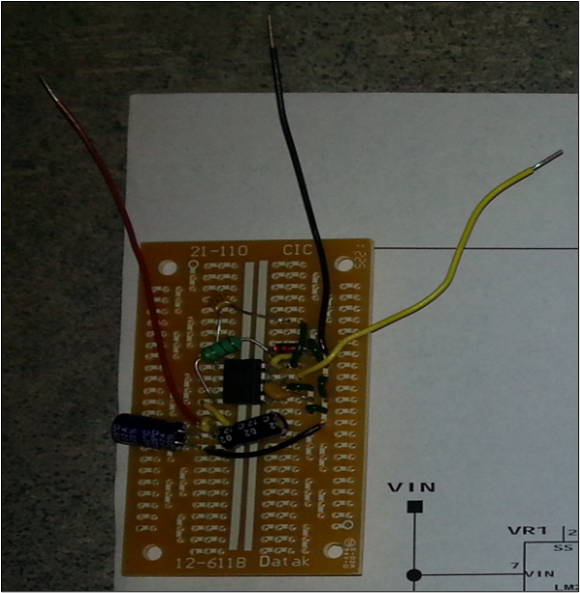
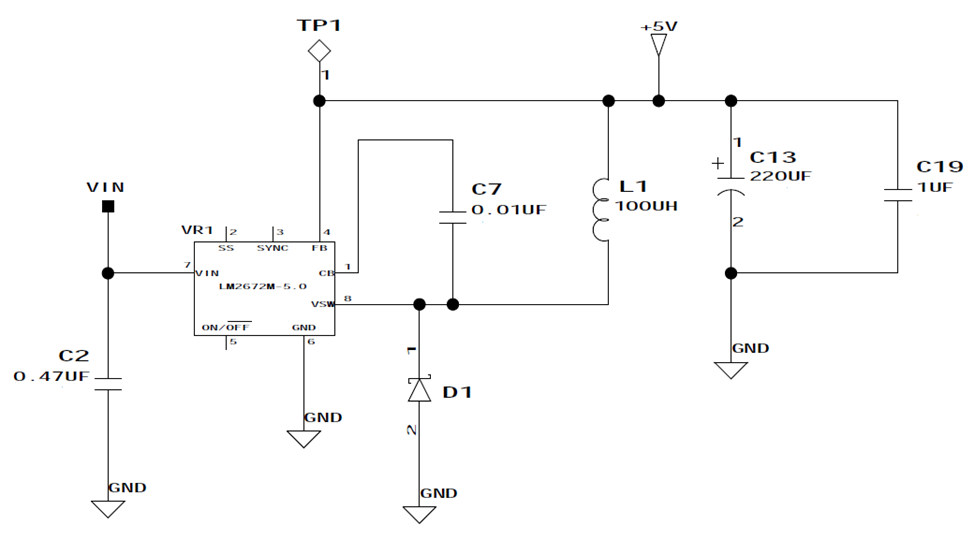
As can be seen in our general system diagram shown in Figure 1, our battery pack is connected to our dsPIC33fj256GP70A DSP. The DSP has an input voltage of 3.3VDC. In order to accommodate this input voltage level, a step down DC-to-DC Buck power converter was built and utilized. The battery pack, with a varying voltage ranging 6.5 – 8.4VDC according to the charge level, was connected to the converter’s input terminal. The output terminal provided a constant 3.3VDC and was connected to the DSP. Our DSP Buck converter was built using a TI-LM2672N-3.3 IC along with other electric components, which can be seen in Figure 8 below. A schematic of the circuit can be found in Appendix A, Figure A1.
Observation Base-Station
Infra-red Receiver
The transceiver will detect the IrDA signal transmitted by the Jumpsuit. The transceiver will utilize the same Vishay IC that the DSP is using. It will automatically decode the incoming IrDA signal and have it ready on the RX port of the IC.
Microcontroller
The microcontroller was used to coordinate the input from the IR receiver and the communication over the Bluetooth channel. We chose the mBed NXP LPC1768 Microcontroller, which is a series of ARM microcontroller development boards. The mBed is a microcontroller that is designed for rapid prototyping with solder-less breadboard, strip-board, and through-hole PCB’s. This microcontroller utilizes an internet based compiler, and included a built-in USB programming interface, which made uploading programs as easy as using a USB Flash Drive. The mBed is C++ based and contains multiple UART ports, allowing various choices for digital inputs and outputs. Bluetooth and IR all communicate via separate UART channels. A class was created to handle the communication between the multiple channels. This class was called the COMM class. As the data was received it was stored within the class. A getter method was used to return each of the three vital signs from the encoded received data. After being received the data was analyzed to determine if the vital sign is considered an emergency situation. The data is then re-encoded and sent through the Bluetooth. This new data string contained three emergency bits, one for each of the vital signs.
Wireless Transmitters
In order to fulfill the radiation free requirement we chose to transmit and display the data by communicating it to an android based device using Bluetooth protocol. In order to add Bluetooth capabilities to our project we found a Bluetooth modem from RobotShop. This specific modem was chosen after considering few other possible options. The features we were reviewing included cost, ease of integration, distance of communication, and reliability. The BlueSMiRF Gold from RobtoShop was chosen because it was fairly cheap (about $65) and it appeared to be an easy module to integrate with our existing system. In addition, this unit was reviewed to be able to transmit up to 350ft in open air with no obstacles.
The BlueSMiRF is small in size (4×1.5cm) and has only 6 inputs/output terminals. In order to integrate the Bluetooth modem we utilized only 4 of the available pins; two pins for the serial (Rx/Tx) communication pipe and two pins for the power and ground.
Power System
The base-station is powered through a wall outlet power cord. It includes an AC-to-DC inverter which takes 100 to 240 VAC from the wall outlet and supplies the base-station electronics with 7.5 VDC at 1A max.
The Base Station’s Microcontroller has an input voltage in a range around 5VDC. In order to reach this input voltage level, a step down DC-to-DC Buck power converter, similar to the one used in powering the jumpsuit’s DSP, was built and utilized. The wall outlet cord is connected to the converter’s input terminal. The output terminal supplies a constant 5.0VDC and is connected to the Microcontroller input voltage pin. The Microcontroller Buck converter was built using the same components as the DSP Buck converter, except it uses a TI-LM2672N-5.0 IC instead. A schematic of the circuit can be found in Appendix A Figure A1.
Integrated Android cell-phone Application
The primary purpose of the base station is to relay physiological and safety information to the android based device. We designed an Android application to allow the user to monitor real time information about the heart-rate, breathing rate, and oxygen levels of the child, as well as featuring safety alarms should a problem with the vitals be detected. These features are visible to the user directly on their android device.
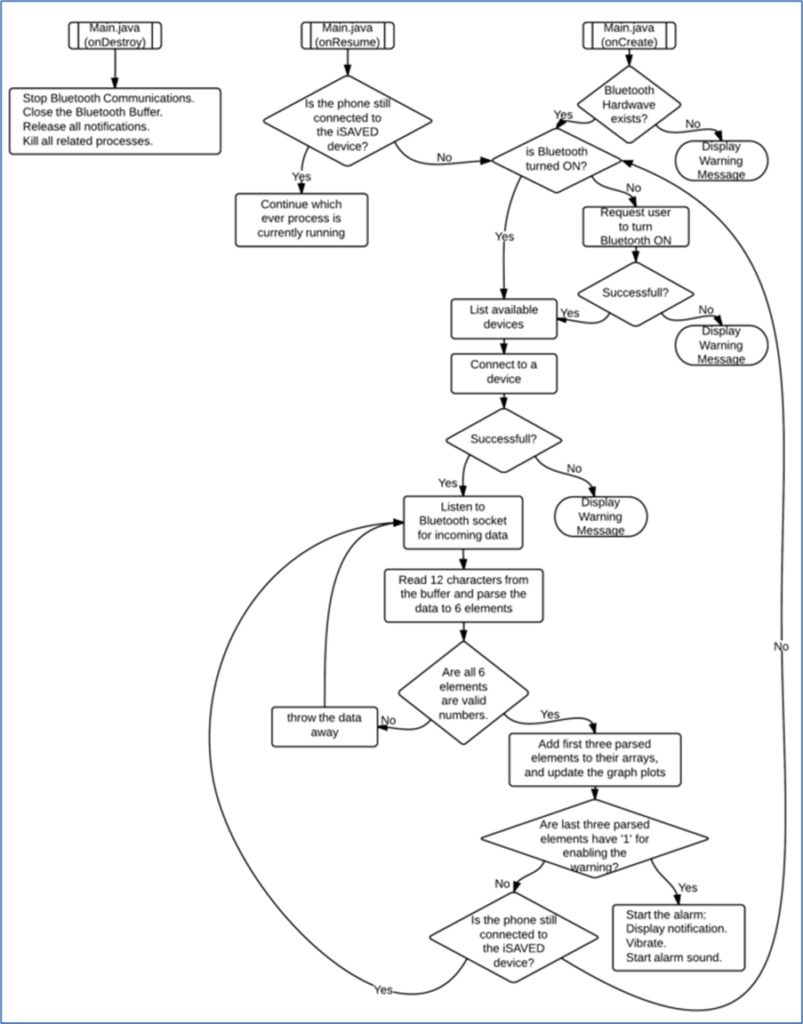
Figure A2 in Appendix A shows the general application flow from start to finish. The application is made of five major parts. Blueetooth communication, data parsing, graphing, notifications,and alarms.
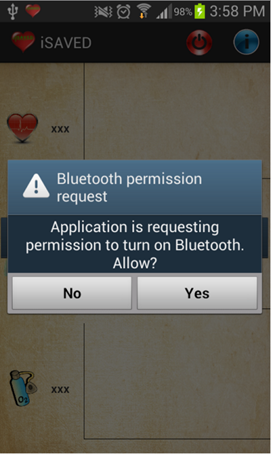
Bluetooth Communication
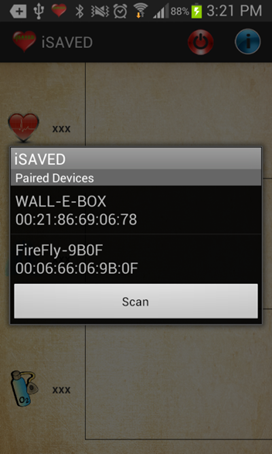
The entire Bluetooth communication is packaged under the main application in two classes: CommandServices and DeviceListActivity. The first file is responsible for the actual Bluetooth communication while the second file is responsible for the searching, and pairing with a device. Once the application starts for the first time it runs the Main class. The main class searches for Bluetooth hardware and inquires whether it is turned on. Once the Bluetooth is turned on, the main class calls DeviceListActivity class on order to start searching for nearby devices and displays the user with a list of the devices. After the user picks the iSAVED device and successfully pairs with it the DeviceListActivity returns to the Main class. The Main class then calls for the CommandServices class in order to open a dedicated Bluetooth socket and listen for incoming data. As it detects incoming data in the socket’s buffer it reads the buffer and sends the data to Main class.
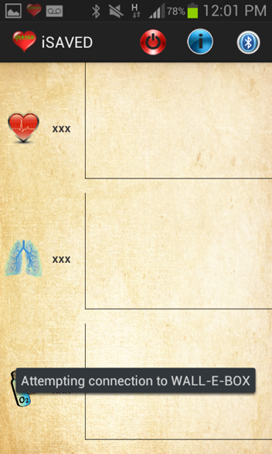
Data Parsing
The Main class then reads only the first 12 characters of the data and parses it data to six segments. The first 3 segemetns are three characters long each and they represet the heart-rate, resperatory rate, and oxygen levels. The last 3 characters in the buffer represent the alarm state of the vital signs. A ‘0’ represents no alarm and ‘1’ represents an alarm state. Once all the data was parsed the application verifies that the received data is in the desired form. If the parsed data is not in the desired format (means the buffer had junk data) it throws the data away and listens for incoming data in the buffer.
Graphing
Once the parsed data was verified, it is added to three arrays; heart-rate, respiratory-rate, and oxygen level arrays. The arrays are then passed to a sophisticated charting engine called AChartEngine. The charting engine plots the updated arrays on a 2D line graph plot.
Notifications
A notification is a message the user can see outside of the application’s normal interface. When a notification is issued, it first appears as an icon in the notification area. To see the details of the notification, the user has to opens the notification drawer. Both the notification area and the notification drawer are system-controlled areas that the user can view at any time. Therefore, in order to fully maximize the utilization of the iSAVED application a general notification appears in the notifications drawer and constantly updates with the parsed data. As a result, the user can send the iSAVED application to the background and check their email, internet, and do anything while the iSAVED application is working in the background. Notifications are also used in displaying the alarms.

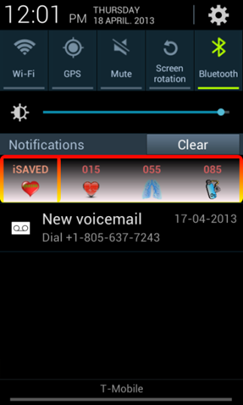
Alarms
If a ‘1’ was detected in one of the three alarm characters, a new notification is created. The notification is displayed in the notification drawer with additional text information regarding the alarm type. In addition, the notification starts a sound alarm and a vibrating sequence in order to alert the parents that they have to check on the baby. Once the notification is dismissed the alarms ends. Aside of creating the notification, the application changes the main graphical view in order to provide additional method of alerting which vital sign trigger the alarm.

Design Evaluation
Initially in our design specifications we planned on using a Texas Instruments DSP mostly based on its speed and power consumption. Over the winter semester we found out about Microchip’s dsPIC’s, a popular and powerful DSP line. Microchip sells many development boards for implementing different dsPIC’s. The dsPIC33F is the DSP we decided on due to the fact it is very fast, 40 million instructions per second, uses low power, and has multiple I2C and UART communication channels.
The UART communication channel was used for the IR transceiver. Implementing the UART communication did not take much longer than we planned. Once communication was established we viewed that data through an RS232 terminal on the computer. The I2C communication channel was for the TAOS color sensor. Due to the fact that none of us have worked with I2C before, this communication channel gave us the most problems. The libraries given to us in the IDE were very low level and setting up the configuration bits correctly proved to be very challenging. Once we got the TAOS color sensor communicating we realized we limited ourselves to using only one sensor. All of the TAOS sensors we bought used the same communication address so stringing multiple sensors on one I2C line would prove impossible.
In our initial proposal we had planned to devote a large portion of the spring semester development time to generating the signal processing algorithms from the IEEE papers cited. Unfortunately building and integrating the hardware took much longer than we expected, which cut into the planned algorithm development time.
We were eventually able to create working drivers for the TAOS color sensor and sample data using the arm band sensor we had created. Unfortunately the data we were able to sample was poor quality, and lead us to believe that we needed to use a larger number of sensors in an array, or replace the sensors with a digital camera. We made an attempt to rework the sensor and DSP to utilize a small digital camera rather than the TAOS sensor, but we did not have sufficient time remaining to complete this task.
In addition to scheduling delays due to implementing the hardware, once we were able to get the data needed to develop and test the algorithms, we found it much more difficult to implement the code on the DSP than we had planned. The algorithm for retrieving the blood oxygen level had been tested using a digital camera and processed using MATLAB; however we found that the algorithm did not work similarly when used with the data sampled from the TAOS sensor. Additionally, as we attempted to implement the algorithms for the heart rate extraction we found that the optimized signal processing libraries provided for the dsPIC were very difficult to work with. Combined with the limited time we had available to program the signal processing algorithms, this difficulty prevented our ability implement working processing on the DSP.
Initially the infrared circuit transceiver and endec was not from the same company. After fixing this incompatibility, our new circuit was based off the recommended circuit from the endec datasheet. This setup merely acts as an infrared communication channel. Due to this, there was no returned data when configuring the endec and the transceiver did not return any data after a successful transmission. With these constraints, unless it worked nothing was shown in the terminal. To troubleshoot each system was checked at the input and output with a logic analyzer. Initially we had a PC sending the data through UART, which then went to the endec, and then to the transceiver. We used the logic analyzer at each of these inputs and outputs to determine if the data was as expected. A break through arose when capacitors were added to the VCC of the transceiver. After this, we were able to communicate between the two devices. We later removed the complication of configuration by tying the BR/D to low, which forces the default configuration.
Our project proposal discussed designing various jumpsuits, primarily focusing on the seasons. For the final product designs for jumpsuits targeted at are created for boys or girls, or for warmer or colder temperatures. It is necessary that the infant is not covered with a blanket, as the IR transmitter and receiver must be in direct line of sight. Therefore, it should be standard that there are several jumpsuits to choose from, depending on the climate that the infant sleeps in, and depending on the sex on the infant. The pouches that encase the electronics, allow for the electronics be removed, but it may be beneficial if the pouches themselves are removable, as well as impermeable. Also, each pouch encompasses a mesh screen to allow for the wireless data transmissions, but research may prove that a more durable material exists that will allow for the wireless transmission of data, and double as a water-resistant protectant.
Our jumpsuit’s electronics core was estimated to draw 50mA while operating. Therefore, theoretically, our 2000mAh battery pack should ensure 40 hours of continuous operation. For testing purposes, we connected our battery to a 50mA drawing resistor, and measured the voltage of the battery every 30 minutes. Figure 16 below shows the obtained plot of the Battery Voltage vs. Time, which can be seen to support the theoretical 40 hours of operation.
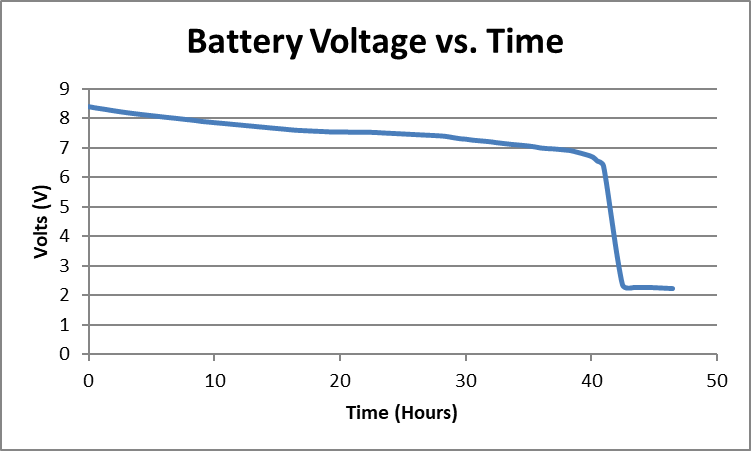
The Adafruit Li-Po USB Charger has 3 indicator LEDs for when it is connected to a USB, when a battery is connected and being charged, and when the battery is fully charged. The charger circuit was tested, and it took around 5 hours to completely charge a fully depleted battery.
The Buck converters, for the jumpsuit’s DSP and the base station’s Microcontroller, were tested by connecting a power supply to the converter’s input, varying the supply’s voltage, and measuring the voltage on the converter’s output terminal. The DSP converter provided a constant 3.3VDC and the Microcontroller converter provided a constant 5.0VDC, for an input range of 6.2 – 12.0VDC, which were perfectly fit for the two major systems, the jumpsuit and the base station.
Design alternatives/improvements for the power systems include:
- The use of the Tenergy 7.4V 1150mAh LiPo battery instead of 2 of the SparkFun 3.7V 2000mAh Li-Po Batteries to form a single battery pack. This will lower the continuous operation period from 40 hours to 23 hours. However, the weight will also decrease from 72g to 47g, and we will be able to cut the costs of 1 battery and 1 charger circuit.
- The use of a AA size 1.2V 1000mAh rechargeable battery. This will require the use of a Boost DC-to-DC converter to step up the voltage from 1.2V to 3.3V, which might prove to be a lot harder to build and implement than the Buck converter used. On the other hand, the weight and the costs will significantly decrease, and these batteries are more available on the market.
- The Adafruit Li-Po USB Charger circuit can be adjusted by soldering in a resistor which will trigger the Fast Charge Mode that increases the charging current and can considerably decrease the charging time to 2–2.5 hours.
In developing the cellphone application, we did not have the sensor connected until almost the end. In order to test the application separately a laptop with a Bluetooth modem was used to send simulated data to the application. In order to send data over the Bluetooth, the laptop used a terminal program called RealTerm. The application went through a few design cycles and a few full restructures. As we learned more about java, and especially java for android we found more methods for controlling and checking various states of the application’s classes and activates. For example, we tried to programmatically control the data flow throughout the entire application life cycle. By doing so we created a very large and complex code, but as we slowly learned more about java for android we realized that most of the complex code can be condensed by using built in classes such as Handlers, BroadcastReceivers, and onActivityResults.
Currently, the application detects many possible errors during its operation. By adding error detection the application became more robust and stable. It works as planned and was tested on a selection of different Android devices (both Android smartphones and tablets) without errors. However, there is one issue yet to be addressed; the application does not generate any error when it is connected to a Bluetooth device but not receiving data for a long period. This is due to the fact that we were waiting to finish programming the base-station. If the entire project would have been finished, we would have been able to estimate how often data should be sent over the Bluetooth – and therefore be able to set a time interval to check if no data has come through and throw an error.
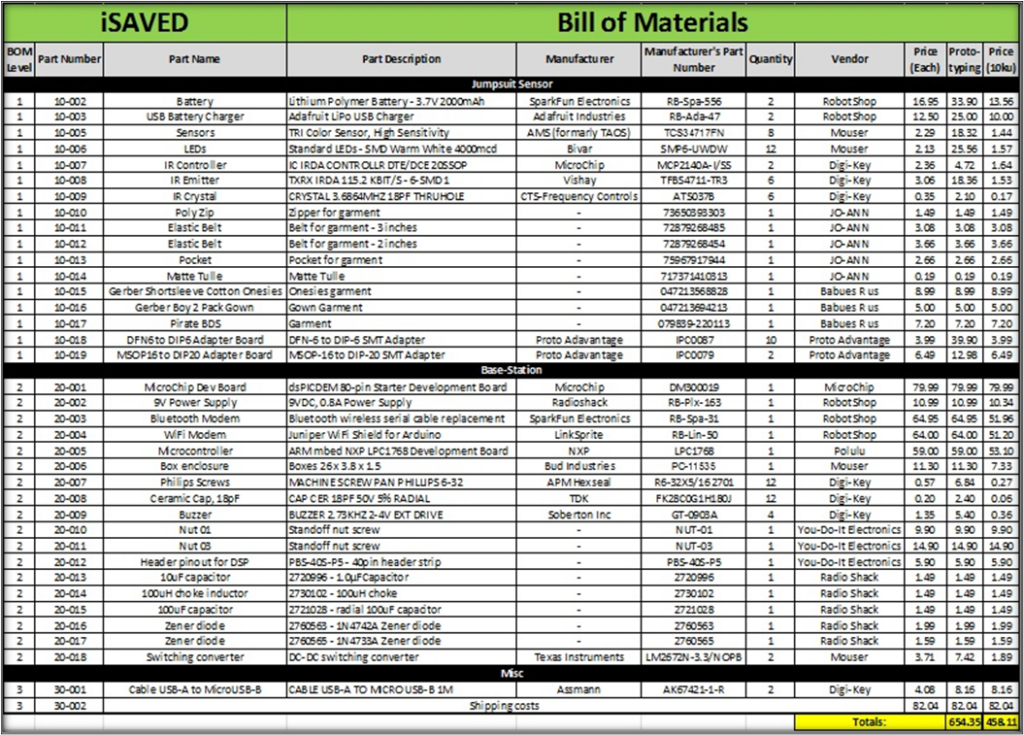
Parts List
We purchased most of the required items from the vendors we chose. Some of the items we purchased at department stores as doing so proved to be more time efficient. The table below lists the prototyping and production costs.
Appendix
| Age Group | Respiratory Rate | Heart Rate | Systolic Blood Pressure | Weight in kilos | Weight in pounds |
| Newborn | 30 – 50 | 120 – 160 | 50 – 70 | 2 – 3 | 4.5 – 7 |
| Infant (1-12 months) | 20 – 30 | 80 – 140 | 70 – 100 | 4 – 10 | 9 – 22 |
| Toddler (1-3 yrs.) | 20 – 30 | 80 – 130 | 80 – 110 | 10 – 14 | 22 – 31 |
| Preschooler (3-5 yrs.) | 20 – 30 | 80 – 120 | 80 – 110 | 14 – 18 | 31 – 40 |
| School Age (6-12 yrs.) | 20 – 30 | 70 – 110 | 80 – 120 | 20 – 42 | 41 – 92 |
| Adolescent (13+ yrs.) | 12 – 20 | 55 – 105 | 110 – 120 | >50 | >110 |
References
| [1] | “Life expectancy at birth (both sexes combined) by major area, region and country, 1950-2100 (years),” April 2011. [Online]. Available: http://esa.un.org/unpd/wpp/Excel-Data/DB01_Period_Indicators/WPP2010_DB1_F05_1_LIFE_EXPECTANCY_0_BOTH_SEXES.XLS. [Accessed 13 June 2012]. |
| [2] | “Infant mortality rate (both sexes combined) by major area, region and country, 1950-2100 (infant deaths per 1,000 live births),” April 2011. [Online]. Available: http://esa.un.org/unpd/wpp/Excel-Data/DB01_Period_Indicators/WPP2010_DB1_F06_1_IMR_BOTH_SEXES.XLS. [Accessed 13 June 2012]. |
| [3] | M. M. Mathews TJ, “Infant Mortality Statistics From the 2007 Period Linked Birth/Infant Death Data Set,” National Center for Health Statistics, Hyattsville, 2011. |
| [4] | National Institute of Child Health & Human Development, “Reduce the Risk of Sudden Infant Death Syndrome (SIDS) – SIDS Facts,” National Institute of Health, November 2000. [Online]. Available: http://www.nichd.nih.gov/sids/upload/PART_II.pdf. [Accessed 13 June 2012]. |
| [5] | Centers for Disease Control and Prevention, “Sudden Unexpected Infant Death and Sudden Infant Death Syndrome,” 30 May 2012. [Online]. Available: http://www.cdc.gov/sids/. [Accessed 13 June 2012]. |
| [6] | Centers for Disease Control and Prevention, “CDC’s Sudden Unexpected Infant Death Initiative,” 10 May 2011. [Online]. Available: http://www.cdc.gov/sids/SUIDAbout.htm. [Accessed 13 June 2012]. |
| [7] | National Institute of Child Health & Human Development, “Reduce the Risk of Sudden Infant Death Syndrome (SIDS),” November 2000. [Online]. Available: http://www.nichd.nih.gov/sids/upload/PART_I.pdf. [Accessed 13 June 2012]. |
| [8] | Babies”R”Us, “Summer Infant Slim & Secure Digital Handheld Color Video Monitor,” Toys”R”Us, [Online]. Available: http://www.toysrus.com/product/index.jsp?productId=3763010#. [Accessed 13 June 2012]. |
| [9] | Babies”R”Us, “Angelcare Movement Sensor with Sound Monitor,” Toys”R”Us, [Online]. Available: http://www.toysrus.com/product/index.jsp?productId=2343185. [Accessed 13 June 2012]. |
| [10] | Babies”R”Us, “Tommee Tippee Closer to Nature Digital Video Sensor Pad Monitor,” Toys”R”Us, [Online]. Available: http://www.toysrus.com/product/index.jsp?productId=12067031. [Accessed 13 June 2012]. |
| [11] | D. B. Hoch, “Cerebral hypoxia,” 13 September 2010. [Online]. Available: http://www.nlm.nih.gov/medlineplus/ency/article/001435.htm. [Accessed 13 June 2012]. |
| [12] | [Online]. |
| [13] | A. Myers, “Apple iPhone 4S vs. Android: iPhone Sales Pass Android Sales in Last Three Months,” 18 January 2012. [Online]. Available: http://www.ibtimes.com/articles/283918/20120118/apple-iphone-4s-vs-android-sales-pass.htm. [Accessed 13 June 2012]. |
| [14] | The World Factbook 2012. Washington, DC: Central Intelligence Agency, 2012., “COUNTRY COMPARISON :: INFANT MORTALITY RATE,” 2012. [Online]. Available: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2091rank.html. [Accessed 14 June 2012]. |
| [15] | M. JA, H. BE, S. PD, V. SJ, M. TJ and O. MJK, “Table 4. Live births, by plurality and detailed race and Hispanic origin of mother: United States, selected years 1970-2008,” 2010. [Online]. Available: http://www.cdc.gov/nchs/data/hus/2011/004.pdf. [Accessed 14 June 2012]. |
| [16] | W. Verkruysse, L. O. Svaasand and J. S. Nelson, “Remote plethysmographic imaging using ambient light,” OPTICS EXPRESS, vol. 16, no. 26, pp. 21434-21445, 22 12 2008. |
| [17] | S. H. Kirk, “Photoplethysmography: Beyond the Calculation of Arterial Oxygen Saturation and Heart Rate,” ANESTHESIA AND ANALGESIA, vol. 105, pp. S31-S36, 2007. |
| [18] | S. H. Kirk, “Photoplethysmography: Beyond the Calculation of Arterial Oxygen Saturation and Heart Rate,” ANESTHESIA AND ANALGESIA, vol. 105, pp. S31-S36, 2007. |
| [19] | M. Aboy, J. McNames, T. Thong, D. Tsunami, M. S. Ellenby and B. Goldstein, “An Automatic Beat Detection Algorithm for Pressure Signals,” IEEE Transactions on Biomedical Engineering, vol. 50, no. 10, pp. 1662-1670, 2005. |
[20] Aboy. M; McNames J; Thong, T; Tsunami, D; Ellenby, M.S; Goldstein, B; “An Automatic Beat Detection Algorithm for Pressure Signals” IEEE Transactions on Biomedical Engineering, Vol. 52, No. 10, October 2005
